Introduction
Venetoclax (VEN), a BCL-2 inhibitor, along with hypomethylating agents (HMAs) has become standard therapy for older patients (pts) with acute myeloid leukemia (AML) not fit for intensive frontline therapy based on recent Phase 3 data reporting a median overall survival (OS) of 14.7 months.
Initially used in CLL, VEN is associated with fatal episodes of tumor lysis syndrome (TLS). Package insert and expert opinion recommendations are for its initiation in the inpatient setting, with a dose escalation of 100mg day 1, 200mg day 2, and 400mg day 3 with IV hydration and close monitoring of TLS markers. In the initial phase 1b trial that resulted in its approval for use in pts with AML all pts were admitted to the hospital for initial venetoclax ramp up and received at least 72 hours of prior TLS prophylaxis, as well as initiation of venetoclax only if the white blood cell count was less than 25,000. No episodes of TLS were documented.
Herein, we evaluated the safety of outpatient VEN ramp up when given in addition to HMAs for the treatment of AML.
Methods
We conducted a retrospective review of pts diagnosed with AML at our institution from 12/1/2016 until 7/1/2020. We identified pts who received HMAs and VEN, either as up-front treatment for newly diagnosed AML or as salvage therapy for relapsed or refractory disease, and stratified pts based on whether venetoclax was initiated in the inpatient or outpatient setting. We then examined baseline AML characteristics including initial blast count, cytogenetics and molecular profiles as well as baseline TLS markers prior to the initiation of VEN. Finally, using the Cairo-Bishop Criteria we examined the number of episodes of laboratory or clinical tumor lysis in all pts. Fisher's exact test and Wilcoxon rank-sum tests were performed to examine differences in categorical and continuous variables.
Results
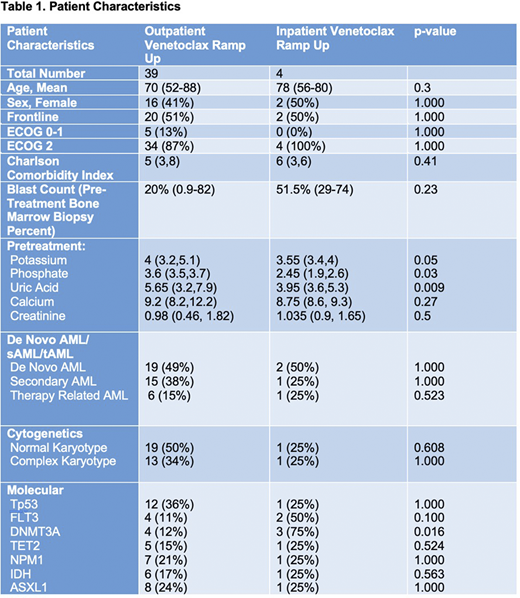
Between 12/1/2016 and 7/1/2020 43 pts at received VEN in addition to an HMA for the treatment of AML (Table 1). 39 pts (91%) had VEN initiation and ramp up in the outpatient setting. Amongst all pts 24 received azacitadine, 11 decitabine, and 8 received both HMAs at some point during therapy. Twenty-two pts received HMA and VEN as frontline treatment while the other 21 received it as salvage therapy. There were 28 pts who received venetoclax within 28 days of starting the HMA, 25 of whom received it as an outpatient and 3 as an inpatient.
Pretreatment labs were notable for median normal values of potassium, phosphate, uric acid, calcium and creatinine (Table 1). The median pretreatment creatinine levels between the two groups were not significantly different. Median pre-treatment WBC count was noted to be significantly higher in the inpatient cohort (37.9 vs 5.5, p-value of 0.01). Cytogenetic and molecular characteristics are included in the table with the only significant difference being a larger percentage of DNMT3A mutation in the inpatient group.
While identification of TLS was somewhat limited by incomplete data on all pts, there was only one identified episode of laboratory TLS (2.5%) with an elevated phosphate and uric acid. This occurred in the outpatient group in a patient whose pretreatment WBC count was greater than 25,000. This pt required admission to the hospital for rasburicase and IV fluids with resolution of the laboratory effects without resultant clinical TLS. There were no episodes of clinical TLS in either group. 30-day mortality from starting VEN was 0% in both groups.
While the Cairo-Bishop Criteria require the presence of 2 lab abnormalities to diagnose TLS we did a further analysis to evaluate for the presence of even a single lab abnormality associated with TLS. We identified 3 additional pts (7.5%) in the outpatient cohort who had the presence of only one lab abnormality associated with TLS within the 7 days after initiating treatment. None of these pts required any further TLS directed treatment or hospitalization.
Conclusion
Our experience with HMAs and VEN showed that outpatient ramp up of venetoclax is safe with a very low risk of laboratory TLS (2.5%) and no evidence of clinical TLS within our cohort. Even with an expanded definition of TLS we only identified 3 additional pts who developed laboratory abnormalities associated with TLS. Our results suggest that, in addition to HMA, VEN ramp up can be safely delivered with monitoring to pts with a WBC count less than 25,000 in the outpatient setting.
Olszewski:Genentech, Inc.: Research Funding; Spectrum Pharmaceuticals: Research Funding; TG Therapeutics: Research Funding; Adaptive Biotechnologies: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal